We make medications more affordable for the people who need them, so they can live their lives more fully.
At Navitus, we are driven by a singular purpose: to improve lives by making medications more affordable. Our team is passionate about reimagining the pharmacy benefit model, delivering solutions that lower costs while maintaining the highest standards of care.
We partner with health plans, employer groups, government programs and other key segments to create customized solutions that put people first.
Member Satisfaction Rate
Navitus is trusted by its members for transparent, affordable, and patient-centered pharmacy benefit solutions.
Lower Medication Costs
Our transparent pricing model reduces prescription drug costs by up to 20% compared to traditional PBMs.
Pass-through Model
All savings from manufacturer rebates and discounts are passed directly to clients—no hidden fees, ever.
Who We Serve
Partnering with You for Better Health and Lower Costs
At Navitus, we serve a diverse range of partners—from patients and members to prescribers, pharmacies, employers, and health plans. Our tailored pharmacy benefit solutions ensure everyone has access to affordable medications, improving health outcomes while driving down costs.
Trusted by Leading Organizations Nationwide
Join the growing list of employers, health plans, and providers who rely on Navitus for transparent, cost-effective pharmacy benefit solutions that improve care and lower costs.
Case Studies

Empowered by Strategic Opportunities and Service Excellence
Putnam | Northern Westchester Health Benefits Consortium (PNW HBC) was the first municipal cooperative…
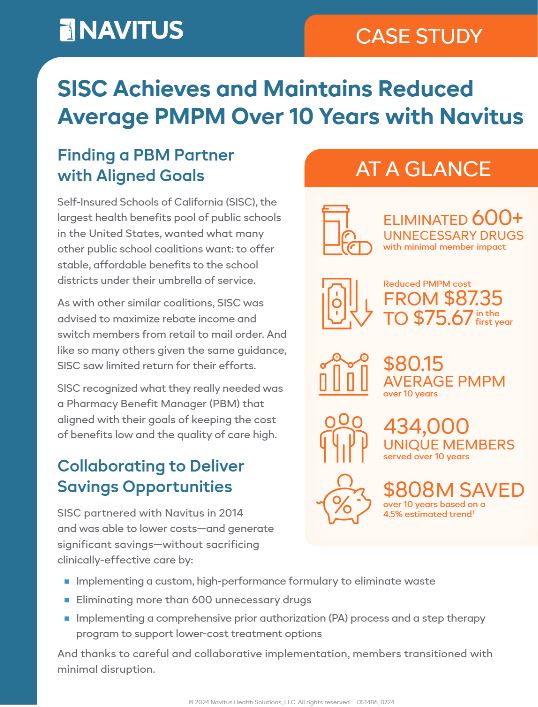
SISC Achieves and Maintains Reduced Average PMPM Over 10 Years with Navitus
Self-Insured Schools of California (SISC), the largest health benefits pool of public schools…




























