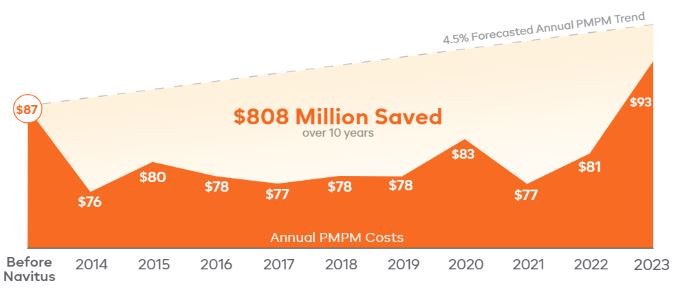
SISC Achieves and Maintains Reduced Average PMPM Over 10 Years with Navitus
Finding a PBM Partner with Aligned Goals
Self-Insured Schools of California (SISC), the largest health benefits pool of public schools in the United States, wanted what many other public schools want: to offer stable, affordable benefits to the school districts under their umbrella of service.
As with other similar coalitions, SISC was advised to maximize rebate income and switch members from retail to mail order. And like so many others given the same guidance, SISC saw limited returns for their efforts.
SISC recognized what they really needed was a Pharmacy Benefit Manager (PBM) that aligned with their goals of keeping the cost of benefits low and the quality of care high.
Collaboration to Deliver Savings Opportunities
SISC partnered with Navitus in 2014 and was able to lower costs—without sacrificing clinically-effective care by:
- Implementing a custom, high-performance formulary to eliminate waste
- Eliminating more than 600 unnecessary drugs
- Implementing a comprehensive prior authorization (PA) process and a step therapy program to support lower-cost treatment options
And thanks to careful and collaborative implementation, members transitioned with minimal disruption.
Delivering Savings Beyond the First Year
SISC saw a 13.4% decrease in total new cost per member per month (PMPM) in their first year—despite the release of new, high-cost medications.
In the decade since, SISC has achieved $608 million in rebates and has had more than 26 million claims processed. More importantly, in an industry where costs continue to increase year over year, SISC has seen minimal increases to its pharmacy benefit costs, with an average total net cost PMPM of $80.15 over 10 years. This is less than their PMPM in 2013.
Ready to lower your pharmacy benefit costs?
Contact us at [email protected].
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








