Rx Money Saving Tips
3 Ways to Lower Your Drug Costs
One out of every three Americans are unable to afford to take their medication as prescribed, and 45% haven’t filled a prescription due to cost.1
Here are a few strategies to help you save on your prescriptions and have a little extra money in your pocket:
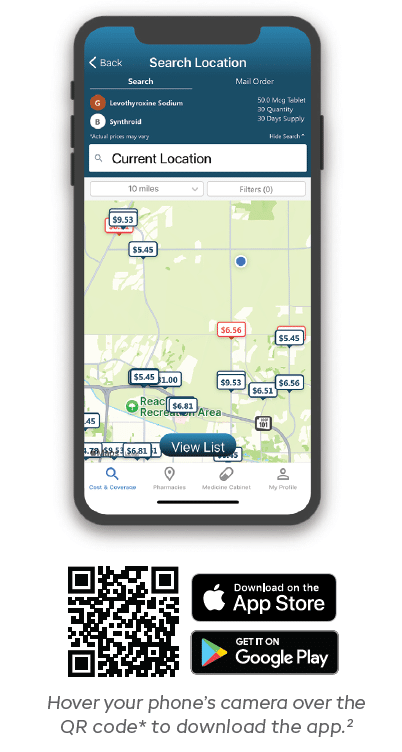
1. COMPARE THE COST OF YOUR DRUGS
Here’s a well-known industry secret: different pharmacies can charge different prices for the same medication. Use the Cost Compare feature in the Navitus member portal to find out which nearby pharmacy offers your medication at the lowest price. It lets you compare prices at local pharmacies as well as by mail order.
2. CONSIDER A LESS-EXPENSIVE GENERIC
Did you know that brand-name drugs can be over 20 times more expensive than the generic equivalent? Generics are just as effective as brand-name drugs, have the same active ingredients and go through the same rigorous U.S. Food and Drug Administration (FDA) testing. If you’re currently taking a brand-name drug, ask your provider if a generic is appropriate.
3. TAKE ADVANTAGE OF CONVENIENT 90-DAY REFILLS
You could make fewer trips to the pharmacy and, in many cases, also save money by asking your prescriber if your maintenance medication can be filled every 90 days instead of every 30 days. Typically, 90-day refills can be filled either at your retail pharmacy or by mail order.3 Check your plan details on the Navitus member portal or your plan’s website.
Sign in to your portal at www.navitus.com/members to access Cost Compare, find generics and more. You can also download the mobile app2 for access on the go.
- Navitus Health Solutions Unpublished Survey, October 2, 2024, 2,000 Americans
- The mobile app, and individual features of the app, may not be available for all benefit plans managed by Navitus, or for every member of each plan. Please refer to your plan for more information. Mobile app registration is simple and secure and may require your member ID. The app is available to iOS and Android users. You must be 18 years or older and currently covered under Navitus’ pharmacy benefit plan. Hover your phone’s camera over the code to download the app. For help registering, contact Customer Care: 844-268-9789. Open 24 hours a day, 7 days a week.
- Please refer to your plan description to see if a mail order program is available to you.
* This QR code may identify your IP/device information. However, your personal and health information is strictly confidential and will not be captured.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.