Improving health Outcomes
Medication Therapy Management
At Navitus, we know that patients with chronic diseases can face greater risks for medication-related challenges such as adherence gaps or potential drug interactions. This can lead to poor health outcomes and higher plan costs. That’s why we developed a medication therapy management (MTM) program, supporting patients with chronic diseases to achieve optimal health outcomes.

Tailored to Plan-Specific Needs
Focused, clinical engagement that supports member health
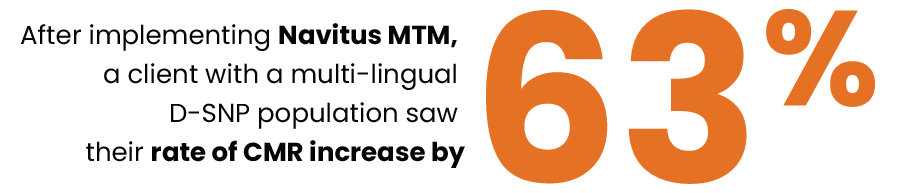
Offered through our Clinical Engagement Center, our customizable, fully CMS-compliant MTM program is built to support Medicare beneficiaries and Part D plans, with the additional ability to support Medicaid and Commercial plans looking to improve patient health outcomes. When implemented for a Medicare plan, the member engagement and clinical support can contribute to improved Part D Star Ratings measures.
Have Questions?
Email us at [email protected] or contact your account team.
MTM OVERVIEW
Optimized, Outcome-Focused Medication Therapy
Clinical pharmacists review eligible participants’ medication profiles and contact the participants via telephone to discuss possible issues or concerns. They also seek to help plans optimize medication therapies for efficacy, safety and cost purposes.
- Cost-effective pricing, so plans pay only when patients participate
- Patient-centric communication with prescribers including a post comprehensive medication review (CMR) fax
- On-demand reporting with customizable formatting and downloadable reports and call logs
Software as a Service (SaaS) Solution
Built By Pharmacists, For Pharmacists
Improved plan-led member outreaches
Our MTM platform can support plan-led interventions. Clinical algorithms are customizable to support member outreach and prescriber engagement with evidence-based recommendations.