PBMI Annual National Conference Recap: The Truth About Transparency
Is your PBM contract truly transparent? Are you looking for a more transparent option? Learn about the latest PBM models and how to assess their levels of transparency.
Today’s employers demand greater transparency, accountability and overall plan performance. Yet, 63% of employers feel that PBMs aren’t transparent, especially when it comes to revenue streams.1 While “transparency” is a term widely used among PBMs, most aren’t truly transparent. Why does this matter? If your PBM isn’t transparent, you may be paying too much.
Earlier last month, Navitus spoke at the Pharmacy Benefit Management Institute (PBMI) Annual National Conference about new PBM models in the marketplace, whether they are truly transparent and what this can mean for your pharmacy benefit plan. In this recap, we will:
Explore how PBMs are using the term “transparency” and what it can mean for your Rx benefit plan
Discover the latest trends in PBM contracts, and how a lack of transparency could be costing you more
Identify the keys to achieving contract transparency with your PBM partner and explore how it can benefit your organization
The Demand For Transparency
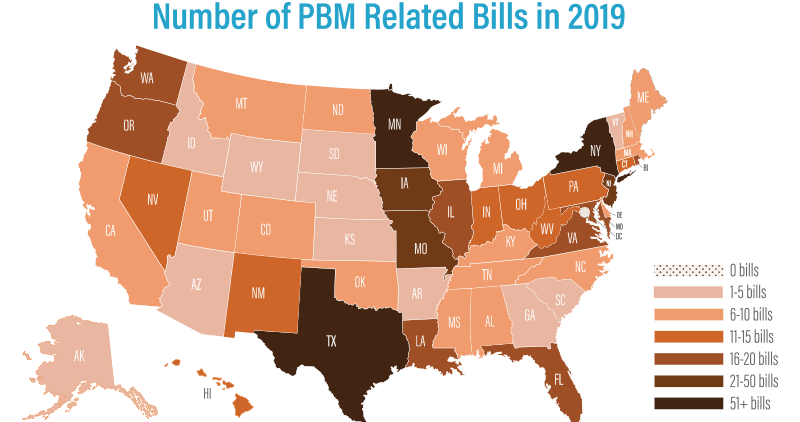
A wide spread lack of trust and skepticism exists for PBM business practices, and only 35% of employers feel that their PBMs are very trustworthy.1 This distrust is often justified. For example, a recent Medicaid report from the state of Ohio uncovered spread of 8.8% between what was billed to plans and what was paid to pharmacies, meaning that the state paid $224 million more than it should have.2 As a result, over 650 bills affecting PBMs were considered in all 50 states and more than 150 bills were adopted.
Many of these bills mandate transparency on MAC lists, PBM pricing and manufacturer drug pricing and limit PBM margins under managed care organizations (MCO) and accountable care organizations (ACO). Others carve out pharmacy benefits from Medicaid programs, regulate pharmaceutical services for dual-eligible and disabled populations and mandate medication therapy management (MTM).
Many states have also considered or passed bills to license and regulate PBMs, requiring annual reports to disclose pricing, drug acquisition costs and rebates. In some cases, these bills also include rules covering network adequacy, gag clauses, claw backs and pharmacy audits. States that have adopted this type of legislation include Florida, Illinois, Louisiana, Maine, Minnesota, New Hampshire, Utah and West Virginia.
Understanding True Transparency
Determining if a PBM is truly transparent is difficult since no industry-wide definition of transparency exists. To achieve true transparency, it is important to view it not as a financial term, but as an operational way of doing business. True transparency includes:
Zero spread on pharmacy or pharmaceutical manufacturer claims
100% pass through of all rebates and discounts, including any upside or increased savings throughout the contract
Formulary product selection based on a lowest-net-cost philosophy, not rebates
Audit rights for all documents, data, network pharmacy arrangements and pharmaceutical contracts
Prior authorization and step therapy that prioritize cost management, not PBM revenue
A single MAC list applied across all distribution channels
Achieving Contract Transparency
A transparent PBM contract is key to making sure you’re not paying too much. Make sure that your contract has clear, concise definitions and gives you unrestricted audit rights down to the claim level, as well as full access to all of your data at all times. A truly transparent PBM will also allow unrestricted access to pharmaceutical manufacturer and pharmacy contracts, so you can confirm for yourself that these contracts are being made with your organization’s interests in mind.
Ultimately, your contract should give you complete control over all aspects of your pharmacy benefit, including network/distribution channels and formulary, as well as the ability to clearly see whether your PBM is minimizing your costs or maximizing their revenues.
A Checklist for Achieving True Transparency
In addition, following the guidelines below will allow you to better assess the transparency of your contract to make an informed decision about whether your PBM is aligned to meet your goals or not.
Evaluate how the PBM earns revenue so you can see where your spend is going
Look at all-in costs versus what you get back in rebates to get a more accurate picture
Get clear definitions of the terms referred to in the PBM contract
Use actual acquisition cost and total all-in drug costs to determine your ‘adjusted AWP starting point’
Look for rebate guarantees that allow you to achieve more savings and avoid rebate guarantee caps
Ensure your contract includes unrestricted full audit rights at the claim level, and establish any associated costs in advance
At the end of the day, your PBM’s level of transparency can have a real impact on your plan performance. Make sure to clarify contract components and definitions to guarantee operational transparency and ensure that your PBM contract aligns with your financial, operational and philosophical goals.
To learn more, check out our e-book, 7 Things You Need to Know About Pharmacy Benefit Management Models.
Toward Better Value: Employer Perspectives on What’s Wrong with the Management of Prescription Drug Benefits and How to Fix it. National Pharmaceutical Council. 2017. www.npcnow.org.
Ohio State Medicaid Report. State of Ohio. 2018.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








