PBM 101: Why the Model Matters
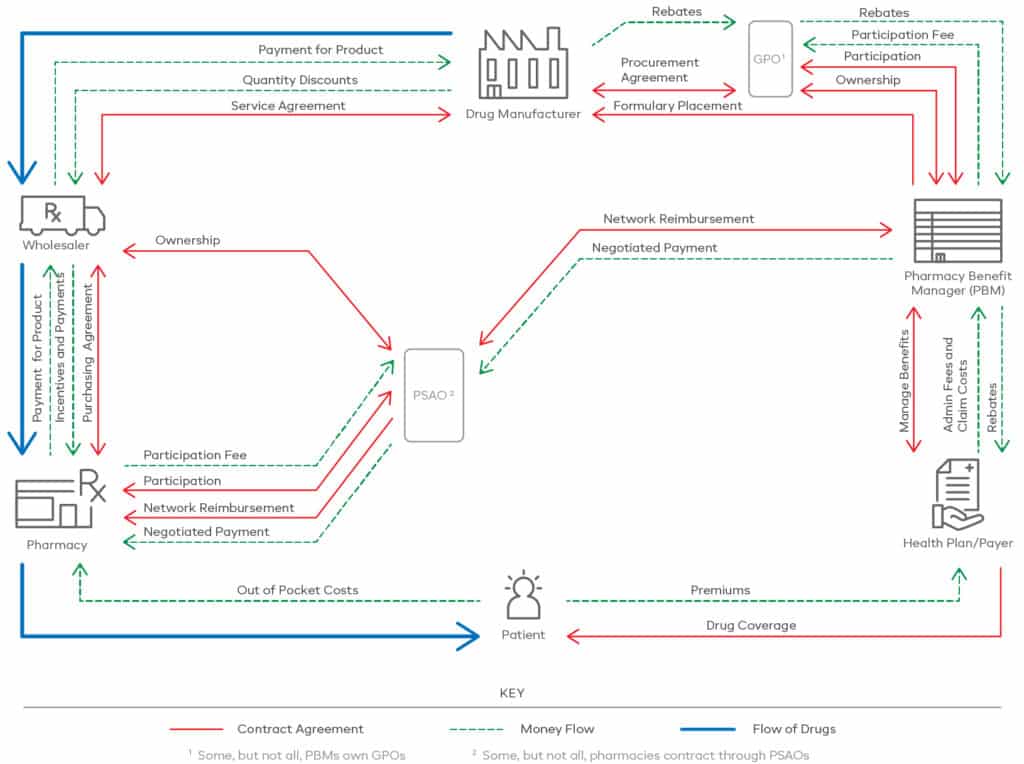
In the pharmaceutical and healthcare industry, pharmacy benefit managers (PBMs) are conduits of expertise, analytics and savings opportunities, poised to deliver exceptional health care while driving down costs. They coordinate between drug manufacturers, pharmacies, health plans and plan sponsors (see the drug supply chain, below). And when any organization takes into account their plan members’ health, not to mention the millions of dollars at stake, choosing a PBM is an important decision.
The Drug Supply Chain
But with so many PBMs out there, falling into a range of PBM models, how does someone choose the right one?
The Three Types of PBMs
There are three conventional PBM contracting models, each of which address complexities within the industry, reacting to obligations for regulatory, health plan and member audience needs and requirements. These complexities include: addressing federal guidelines, lowering drug spend, managing specialty care and medications, and improving access and adherence.
Traditional Model –These PBMs offer volume discounts and high rebates to achieve cost savings. However, they often retain spread compensation from pharma revenue on rebates, discounts and incentives, leading to little or no transparency into their business practices.
Hybrid Model – Bridging the gap between traditional and pass-through PBMs, hybrid model PBMs offer some transparency into pricing and revenue business practices, and they may also charge an admin fee.
Pass-through Model – As the most transparent of the PBM models, pass-through PBMs, such as Navitus, pass 100% of all rebates and discounts back to the plan sponsor. They may also offer additional member health improvement options, like adherence programs, specialty care and medications, and non-drug treatments.
Want to learn more about the three PBM models and how they work? Read more in our blog post: The Three PBM Models.
Why The Pass-through Model is Better for You
If we had to point to one reason why Navitus was created to be a separate pass-through solution, instead of even considering traditional or hybrid, it would be transparency. The pass-through model offers the clearest view of where money is going and what costs actually cover in a health plan. But even then, some PBMs are able to play fast and loose with the parameters of the model, which is why we don’t only rely on the model itself to decide how our business works.
Here are some of the things Navitus as a company does to enact meaningful change:
Rebates – We return 100% of all manufacturer rebates back to our clients, including all ongoing network rate and rebate improvements, and all pharma-related dollars.
Transparency – We provide full financial and operational disclosures, 100% audit capabilities at the claim level and 360 degrees of financial transparency, with no hidden revenue streams.
Spend – We lower overall drug spend and cost-of-care and have proven year-over-year lowest-net-cost trend management.
Adherence – We improve medication adherence and member health through evidence-based clinical programs and robust adherence programs, with a strong focus on member satisfaction.
Non-drug Solutions – We offer alternative treatment options that can reduce long-term drug reliance.
At the end of the day, the model is like the frame of a house. It gives a PBM structure, stability and space to grow. How a PBM builds on it from there is up to them.
Ready to learn more about how we’ve built upon the pass-through model to best support your business? Reach out to [email protected].
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








