Navigating the Drug Supply Chain: What You Need to Know
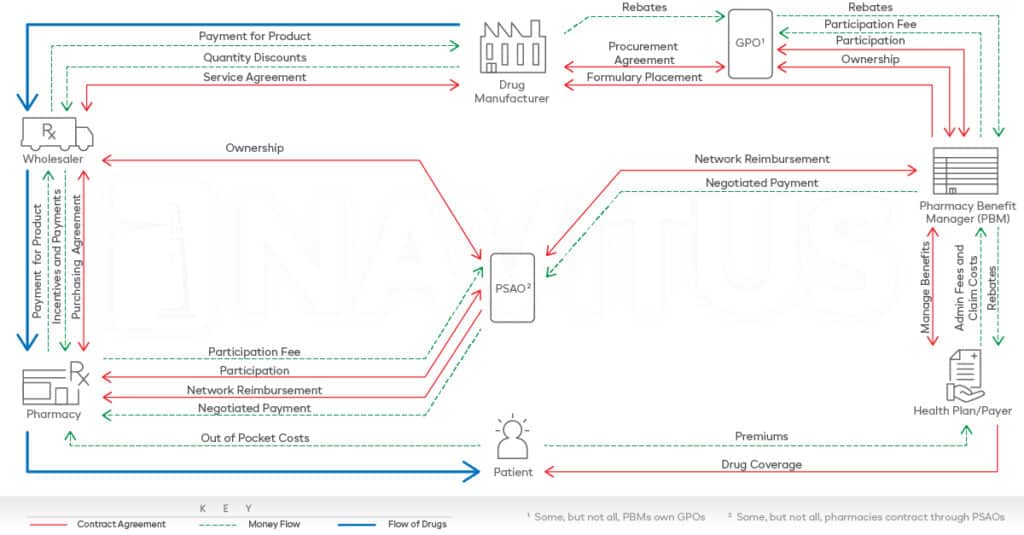
Before a prescription ever reaches a pharmacy counter, it has already moved through a complex ecosystem known as the drug supply chain. From manufacturers and wholesalers to pharmacy benefit managers (PBMs) and pharmacies, each entity plays a role in determining how much a drug costs and who ultimately pays for it.
For plan sponsors, health plans and consultants, this system often lacks transparency, making it difficult to see where the money goes or why medication costs continue to climb. At Navitus, we believe transparency is the foundation for driving better outcomes. That’s why we’re committed to demystifying the supply chain and offering a different kind of PBM experience – one that’s 100% aligned with client goals.
Defining the Drug Supply Chain
In simple terms, the drug supply chain represents the full journey a prescription medication takes from lab to patient. But it’s not a straight line – it’s a complex web of players and financial exchanges that happen behind the scenes.
While the basic structure of the supply chain is consistent across the industry, how a PBM operates within it can significantly impact cost and care outcomes.
Key Players in the Supply Chain
Each stakeholder plays a specific role, and together they shape drug costs, access and member experiences. Here’s an overview of who’s involved in the drug supply chain and what they do:
Drug manufacturers – They research, develop and produce medications. They also set the list price for each drug, which becomes a starting point for rebate negotiations and pricing strategies across the supply chain.
Group purchasing organizations (GPOs) – These entities help healthcare providers and pharmacies negotiate lower medication pricing by pooling their purchasing power.
Wholesalers – They buy medications in bulk from manufacturers and distribute them to pharmacies and health systems.
Pharmacy services administrative organizations (PSAOs) – These organizations support independent pharmacies by handling administrative tasks and negotiating with PBMs and payers on their behalf, helping them stay competitive.
Pharmacy benefit managers (PBMs) – PBMs act as coordinators between manufacturers, plan sponsors, pharmacies and patients. They negotiate drug prices and rebates, manage formularies, build pharmacy networks and work with plan sponsors to structure benefits that balance cost, access and quality of care.
Health plans/Payers – They partner with PBMs to define which drugs are covered on formulary and how much members will ultimately pay.
Pharmacies – They dispense medications, educate patients and ensure safe, timely access to treatments. PBMs work closely with pharmacies to build strong networks that support both patient access and plan performance.
Patients – They are the reason the entire drug supply chain exists. Yet their experience – how much they pay, how quickly they get their medications and what options they have – is shaped by decisions made long before they reach the pharmacy counter. As a PBM, we never lose sight of that. Every decision we make is to lower drug costs and improve outcomes for people who rely on their medications every day.

How Navitus operates differently within the supply chain
PBMs are at the heart of the drug supply chain, connecting drug manufacturers, payers, pharmacies and patients. But not all PBMs operate the same way. While traditional PBMs often profit from hidden fees, spread pricing and retained rebates, Navitus takes a fundamentally different approach. As a 100% pass-through PBM, we are structured to serve the best interest of plan sponsors and their members.
Here’s what sets us apart:
100% of rebates and discounts go back to plan sponsors – All rebates and discounts secured from manufacturers are passed entirely to the plan sponsors. Navitus does not retain any portion.
Full transparency across the chain – Plan sponsors receive complete visibility into contract terms, rebate arrangements and claim-level data – enabling better oversight and accountability.
No spread pricing – We do not profit from the difference between what is paid to the pharmacy and what is billed to the plan sponsor. Pricing is clear and consistent.
Aligned incentives – Our model is built on lowering drug costs and improving access. With no financial gain tied to inflated drug prices or hidden rebates, our interests are aligned with plan performance and member well-being.
The Bottom Line
You don’t have to navigate the drug supply chain blindfolded. With the right PBM partner, you can gain the clarity and control you need to manage costs and care effectively.
Ready to see how our model works in real life? Explore our PBM 101 series for more insights or connect with our team at [email protected] to learn how Navitus can help build a pharmacy benefit that works for your organization.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.