How Digital Health is Enhancing Pharmacy Benefits
Digital health has exploded in popularity with COVID-19. Find out how digital health works, how it can benefit members and what Navitus has to offer.
What is DIGITAL HEALTH?
Digital health is the use of digital tools to deliver health care and improve health. According to the US Food and Drug Administration (FDA), it includes mobile health, health information technology, wearable devices, telehealth, telemedicine and personalized medicine.1
While there has been growing interest in digital health over the last few years, the COVID-19 pandemic has led to a sharp increase in interest. In fact, digital health is one of the few industries to have grown during the pandemic, with companies receiving $6.3 billion in funding in the first half of 2020, a 24% increase over 2019.2 While much of this interest has been in telehealth, which connects members with health care providers remotely, another area that promises to transform health care is digital therapeutics.
Digital Therapeutics Can Benefit Plan Sponsors
Digital therapeutics is a subset of digital health that uses software, apps or other digital technology to manage or treat chronic conditions by changing member behavior. Digital therapeutics differ from widely available wellness apps in that they are backed by rigorous clinical evidence and must be reviewed or approved by regulatory bodies to support product claims of risk, efficacy and intended use. Because of this, plan sponsors that make these programs available know that their members can benefit from substantive improvements in their conditions, leading to fewer complications or hospitalizations and reduced health care costs for both the member and the sponsor. Examples include apps that provide health coaching or assist with exercising or medication monitoring.
Our digital Health Solutions
As part of our commitment to improving member health, we offer an extensive suite of evidence-based digital therapeutics programs to help members manage a range of conditions. All of the programs we offer are fully vetted by our team of clinical professionals to ensure they produce meaningful results. They include the following:
BlueStar®
Designed by experts, educators and physicians, BlueStar supplements existing diabetes care and is prescribed by a health care provider. It helps members manage diabetes and supports adherence to medications used to treat diabetes.
Through the mobile app, members enter their blood glucose readings, exercise, diet and current medications. This information can be shared electronically with the patient’s prescriber. Timely and efficient tracking of the patient’s health status enables prescribers to make better-informed decisions that can lead to improved patient outcomes.
BlueStar can reduce A1C levels and decrease hospital and emergency room visits by up to 58%.

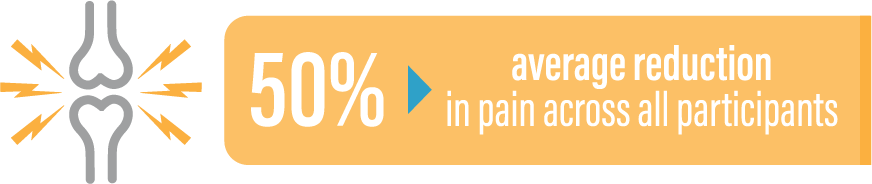
Kiio®
Kiio is a physical therapy, educational and care management mobile app that can reduce lower-back pain through evidence-based exercises. It provides a positive, proactive alternative to prescribed opioids and may also reduce more costly medical interventions, such as surgery, MRIs or injections.
With Kiio, members are assigned tailored exercises that continuously evolve based on user feedback. Members can also access individualized care that includes:
Home exercise programs with accompanying video
Education on overcoming pain
Virtual coaching
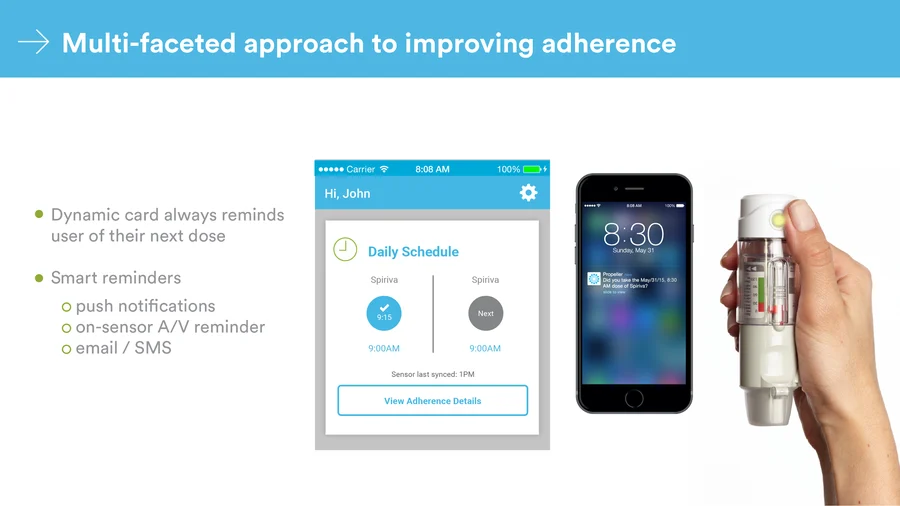
Propeller®
Propeller is a comprehensive digital platform for respiratory health management that combines on-device sensors for inhalers, mobile apps and patient management services for care teams. It can reduce the overuse of rescue inhalers and increase adherence to controller medications for asthma and COPD.
Evidence shows that Propeller can reduce rescue inhaler usage by 79% in one year. In addition, it can save plan sponsors approximately $900 per member per year in direct asthma costs for members with uncontrolled asthma.
Sempre Health
Sempre, an SMS-based engagement program, allows eligible Navitus members to earn discounts on their prescription copays by taking their medications as prescribed. It lowers copays when members fill their prescriptions consistently and on time, reminds members when it’s time for a refill and can even submit refill requests on the member’s behalf.
As members enroll, their copay discounts will be immediately available on eligible medications at the pharmacy they normally use. If members elect to refill elsewhere, they can show their pharmacist a text from Sempre to take advantage of the program discounts. Each time members refill their eligible prescription on time, their discounts can grow—saving them an average of 45% per year on their annual prescription costs and improving member adherence by 15-19%.

For more information on our digital health solutions, contact your account manager or email [email protected]. For more about our clinical care model, visit www.navitus.com/clinical-care-model.
Sources:
- Digital Health. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/digital-health. Updated June 30, 2020. Accessed July 21, 2020.
- Pifer R. Digital health funding shatters records with $6.3B in 1st half of 2020. Healthcare Dive. https://www.healthcaredive.com/news/digital-health-funding-shatters-records-with-63b-in-1st-half-of-2020/581561/. Published July 14, 2020. Accessed July 21, 2020.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Examining Trends that Drive Informed Decisions
Now Available: 8th Annual Drug Trend Report
See the latest results and access industry insights you need to navigate current trend drivers.








