5-Levers to Maximize Plan Performance
Is your PBM maximizing your Rx benefit plan performance and lowering your pharmacy spend? Make sure your PBM is working for you and take your Rx benefit savings to the next level.

With prescription spend for commercial plans projected to grow an average of 5% annually, finding ways to cut costs is more important than ever.1 Here are five levers your PBM can pull to get you on the road to improved plan performance and greater savings.
Lever 1 — The benefit of a true Pass-Through Business Model
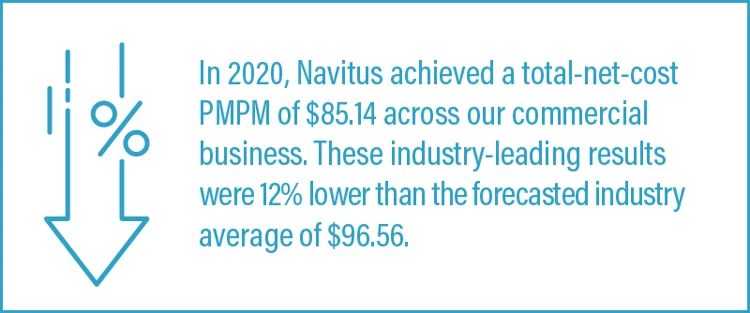
As a plan sponsor, you have specific goals for your drug benefit plan. A PBM with a pass-through business model will align with your goals, focus on the lowest net cost and provide full transparency. With Navitus, all discounts, rebates and fees received are passed along to the plan sponsor. Plan sponsors also benefit from greater flexibility for making edits or changes to plan design, and complete visibility into pharmacy spend. Not sure how your PBM compares? Look at the per member per month (PMPM) pricing. It measures your total pharmacy costs by considering everything that contributes to your bottom-line expenses.
Lever 2 — Lowest-Net-Cost Driven Formularies
Ensuring that you have the right drug mix on your formulary can help your bottom line. A high-performance, lowest-net-cost formulary focuses on clinically sound, cost-effective alternatives, such as generics or less-expensive brands. For example, Navitus’ business model does not chase rebates on high cost drugs; instead we aim to provide you with the lowest cost, choosing rebates only where they make sense.
Lever 3 — Appropriate Utilization MANAGEMENT
Utilization can have a significant impact on your drug trend. Implementing utilization management (UM) tools can help get the right medications into members’ hands. Typical UM tools include prior authorization (PA), step therapy (ST) and quantity limits (QL), to name a few. While most plan sponsors will incorporate PA as part of their UM strategy, PBM models vary and can produce different results. For example, a pass-through PBM business model may recommend lower-cost alternatives based on clinical guidelines to optimize approval rates. Conversely, a traditional PBM that may be earning revenue from PA approvals and could have higher approval rates based on looser criteria.
Lever 4 — Narrow Network Savings Opportunities
As pharmacy benefit costs continue to increase, plan sponsors are increasingly looking to include narrow networks in their benefit management strategies. By limiting the number of pharmacies that participate a narrow network, PBMs can offer plan sponsors deep discounts. And with a pass-through PBM, any discounts received are passed through to the plan sponsor. Plan sponsors that adopt a narrow network strategy typically save between 3-5% off retail drug spend, with some saving as much as 10%.2 A well-designed narrow network will also continue to offer excellent access to members, including both major chains and independent pharmacies.
Lever 5 — High-Touch Specialty Pharmacy
Specialty drugs are high-cost ticket items for plan sponsors and could represent almost 50% of total drug spend. A high-touch specialty pharmacy can help manage specialty drug spend. Navitus’ full-service specialty pharmacy, Lumicera Health Services, is a key example, combining a patient-centered approach with aggressive formulary management, utilization management and waste monitoring. Lumicera’s unique acquisition cost-plus pricing model combined with first-in, first-out (FIFO) methodology works to keep costs in check. And, plan sponsors receive near real-time price adjustments, meaning they benefit from lower-cost medications when they become available.
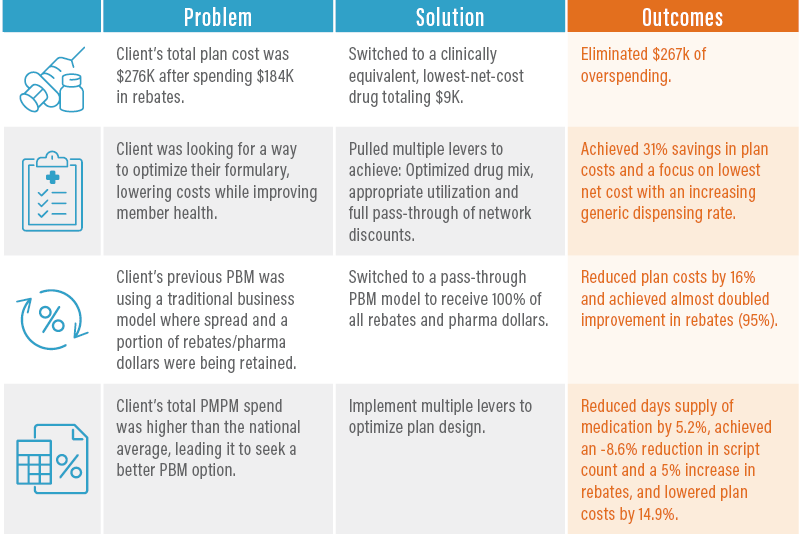
Significant Savings are Achievable
Below are examples of how clients have achieved significant plan savings with Navitus using the multi-lever approach outlined above.
partnering with Navitus
Partnering with Navitus offers you the opportunity to implement strategies that can control your drug spend without trading your organizational goals to maximize plan performance. Although many PBMs promise savings, only Navitus proactively manages your Rx costs by using a multi-lever approach to help you get the results you are looking for. To learn more, contact us at [email protected] or download our e-book: 7 Things You Need to Know About PBM Models.
Minemyer P. Health spending is likely to grow by 5.4% per year through 2028. Here’s why. Fierce Healthcare. https://www.fiercehealthcare.com/payer/cms-actuaries-say-health-spending-likely-to-grow-by-5-4-per-year-through-2028-here-s-why. Published March 24, 2020. Accessed August 12, 2021.
Navitus Internal Data Analysis.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








