Customer Attitudes Around Prescription Drug Pricing and the Role of Pharmacy Benefit Managers
The costs for prescription drugs keep rising, which puts pressures on the wallets of Americans, and more importantly has a potentially devastating impact on our health. Recent reports have found that 1 out of every 3 Americans are unable to afford to take their medication as prescribed, which echoes the latest research from Navitus Health Solutions, which recently polled 2,000 Americans on their attitudes around drug pricing and awareness of the issues impacting pricing. Notably, 48% reported that the price of medication had affected their ability to get a medicine they needed at least once.
Across the board, the survey unveiled that a surprising number of Americans struggle to pay for the medications they need to stay healthy. Surprising findings included:
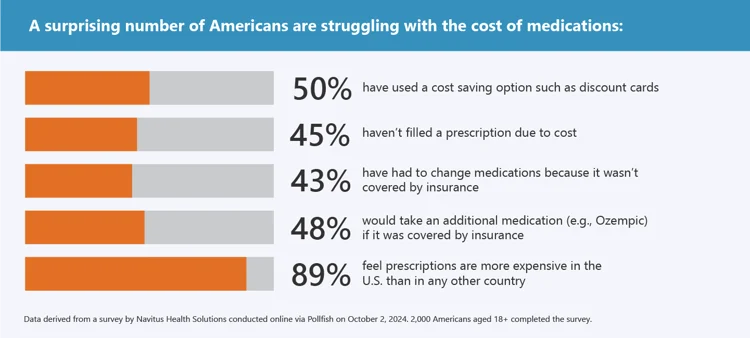
HOW AMERICANS ARE COPING WITH RISING DRUG COSTS
Recent research found that Americans pay, on average, 2.8 times more for prescription drugs than the 33 other countries studies, and 4.2 times more for the larger name-brand drugs. To manage these rising drug costs, Americans are taking things into their own hands to get access to biosimilars and other lower cost medication.
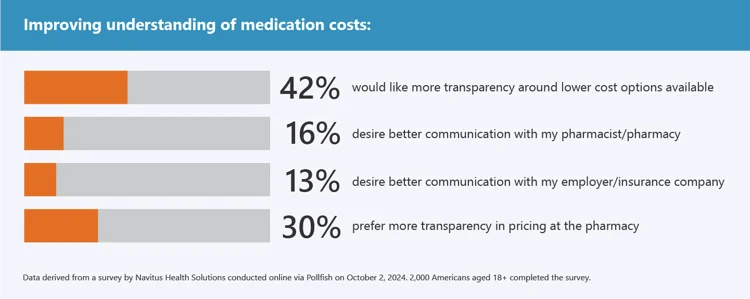
UNDERSTANDING THE COST-MITIGATING FACTORS
Due to these unsustainable rising costs, 88% of Americans stated they believe prescription drug pricing should be a priority for the next administration, and 42% wanted more transparency around lower cost options that are available. However, the survey results, across the board, revealed that Americans are largely unaware of one of the biggest factors impacting drug pricing — pharmacy benefit managers (PBMs).
Over 275 million Americans are served by a PBM, which act as intermediaries in the healthcare system designed to help negotiate discounts and pricing with drug manufacturers. Despite PBMs’ direct influence on drug pricing, the survey found that:
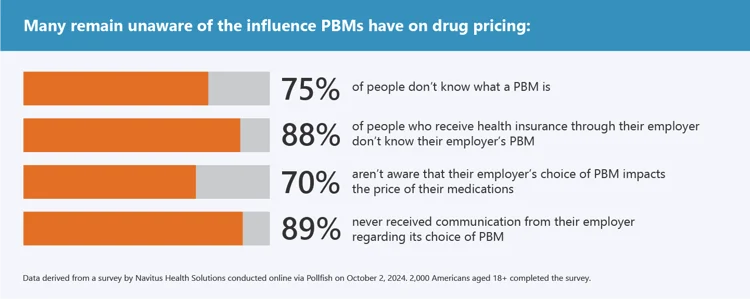
“Despite all recent negative media attention around traditional PBMs, which fill 94% of prescriptions in the U.S., the average American isn’t aware of how these companies operate,” said David Fields, CEO of Navitus Health Solutions. “The traditional PBM model generates profit by creating margin within the drug supply chain. Consumers are commonly unaware and uninformed about the impact of those actions on prescription drug prices accessed through their insurance. American healthcare consumers want lower prices. Healthcare consumers and political leaders want transparency. Innovation to this end is what the Navitus PBM has championed for over twenty years. Not all PBMs are alike. Ours is meaningfully driving lower cost and enabling transparent drug pricing while others are continuing to conspire to keep drug prices high for their benefit. “
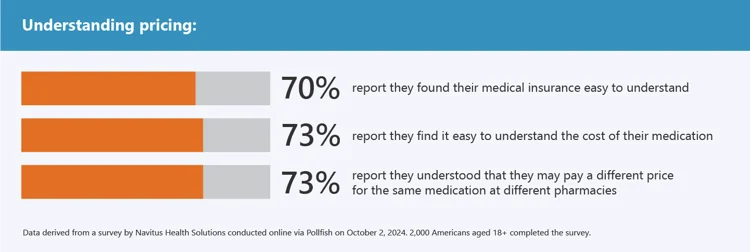
AMERICANS TO PLAY AN INCREASING ROLE IN ADVOCATING FOR LOWER PRICES
“While more consumer awareness around the role PBMs play in prescription drug pricing is vital for real change, I think it’s promising that the majority of respondents understand the variable nature of prescription pricing,” said Sharon Faust, Chief Pharmacy Officer at Navitus Health Solutions.
“People are looking for more transparency and are open to biosimilars and lower cost options,” said Sharon. “If you are concerned about the cost of medication, speak up. Not just to your doctor or pharmacist, but also to your benefits manager if you receive healthcare through an employer.”
SURVEY METHODOLOGY
The data was derived from a survey by Navitus Health Solutions conducted online via Pollfish on October 2, 2024. 2,000 Americans aged 18+ completed the survey.
Of the respondents, 56% identified as female and 43% as male. 93% reported having medical insurance. All decimals in this report are rounded to the nearest percentage point, which may lead to certain numerical totals adding up to slightly more or less than 100%.

MORE ABOUT DAVID
David Fields is the President and CEO at Navitus Health Solutions. He provides enterprise leadership and strategic direction for Navitus, collaborating with the executive management team to maintain Navitus strategic plan and to develop and direct its goals, policies and execution. David has held leadership positions on a number of boards, including the American Heart Association, American Red Cross, Labor-Management Council and the National Conference of Christians and Jews.

MORE ABOUT SHARON
Sharon Faust is the Chief Pharmacy Officer at Navitus Health Solutions. She oversees Health Strategies, Provider Services and Lumicera Health Services. She is a licensed pharmacist in Wisconsin and is on the Board of Directors for the National Association of Specialty Pharmacy and the Drug Selection Advisory Committee for CivicaScript®. In 2023, she was awarded the top 50 most influential leaders in Pharmacy award presented by the Pharmacy Podcast network.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








