How COVID-19 Shaped Prescription Drug Use in 2020
The rapid spread of COVID-19 last year had a profound impact on all aspects of life, including prescription drug use. Find out how changes in policies and behaviors led to shifts in drug utilization in 2020.
In early 2020, during the beginning of the COVID-19 pandemic, we saw dynamic shifts in prescription drug utilization. These changes stemmed primarily from shelter-in-place policies that were established by state and local governments. Further shifts would arise from both the upheaval caused by the pandemic and the ripping effects of the initial shifts.
The following are some key highlights of how COVID-19 changed prescription drug use last year.
Fewer medications were filled for acute conditions
The COVID-19 pandemic moved quickly in early 2020, with the World Health Organization (WHO) first announcing disease’s existence on January 9 and the first American case being reported on January 20. The United States declared a public health emergency by February 3 and a national emergency on March 13, two days after the WHO confirmed COVID-19 to be a pandemic.1 Shortly afterwards, many states and counties enacted shelter-in-place policies to limit the spread of the disease.2
Between policies limiting travel outside of homes, reduced hours for in-person care at doctors’ offices and safety concerns over visiting medical facilities, providers saw a significant decrease in visits. As a result of these factors, Navitus saw a 2.3% overall reduction in medications filled for acute conditions, illnesses that generally develop suddenly and last over a short period of time.
MAINTENANCE MEDICATION UTILIZATION INCREASED
Despite the decrease in medications filled for acute conditions, Navitus’ commercial population saw an overall increase in utilization at the start of the pandemic in March. Driven almost exclusively by maintenance medications, this increase was largely a result of pandemic lockdowns and short-term strategies to ensure adherence and uninterrupted access to prescription therapies. These strategies included temporarily extending prior authorizations, authorizing early refills and increasing fills at retail pharmacies from 30 to 90 days, all of which drove the utilization rate.
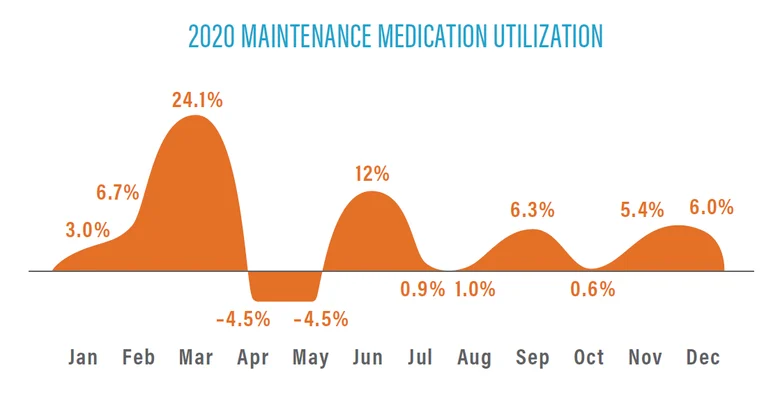
While there was an initial 3% shift from retail to retail extended supply channels, utilization tapered off in April and May, with members remaining at home and using the 90-day supplies they filled in March. Our specialty pharmacy, Lumicera® Health Solutions, closely tracked patient supply and market supply to avoid stockpiling. Smaller increases in utilization followed in June and September as members collected additional 90-day supplies of their medication. Utilization eventually returned back to normal in November and December.
All in all, 62% of scripts filled in 2020 were for maintenance medications, up 2.2% from the previous year.
Behavioral drug use increased significantly
In addition to the disease itself, the COVID-19 pandemic and its resulting economic impact had a significant effect on mental health for many. According to the Kaiser Family Foundation, 4 in 10 adult Americans consistently reported symptoms of anxiety disorder and/or depressive disorder during the pandemic, up from 1 in 10 in previous years.3 Moreover, polling in July 2020 found that 36% of Americans were having trouble sleeping and 32% were having trouble eating.3
Unsurprisingly, these changes resulted in increases in behavioral drug use. We found that behavioral therapy utilization increased by an average of 7.7% last year, with utilization growing as the pandemic progressed. In particular, utilization of anti-depressants increased by 6.6%, anti-anxiety medications saw an 8.7% increase, and anti-psychotic/anti-manic agent use increased by 7.9%.
MEMBERS RECEIVED MORE FLU VACCINES AT PHARMACIES
In order to reduce the burden on health care systems overtaxed by COVID-19, the Centers for Disease Control and Prevention (CDC) made significant efforts to increase flu vaccination for the 2020-2021 flu season. This included making available 11.3 million more doses of the vaccine than in the previous year and undertaking additional education outreach and digital campaigns.4 By all accounts, 2020 proved to be a record year for flu vaccinations, with 189.4 million doses distributed by mid-December, compared to 174 doses in the entire 2019-2020 flu season.5 Although we do not yet have the final number of doses administered, manufacturers anticipated producing 194 to 198 million total doses for the season.4
In total, we found that the number of vaccine scripts filled increased by 52% last year, with the vast majority of that increase attributable to the flu vaccine. This was driven in part by the increase in utilization described above, but also by a shift in where the vaccines were administered. While many vaccines were previously administered under the medical benefit at doctors’ offices or hospitals, the aforementioned reduction in provider visits resulted in members getting their flu vaccines at pharmacies, moving those vaccinations to the pharmacy benefit.
OVERCOMING CHALLENGES
Despite the past year’s challenges, our proven pass-through PBM model kept clients on the path toward measurable savings. Navitus clients paid 12% less than the forecasted industry average and almost a third of our established commercial clients experienced a negative PMPM trend compared to the previous year. We are proud to have achieved another year of significant results for our clients during these unprecedented times, delivering real results that grow over time to create long-lasting value. As we look to a brighter future, we’ll continue to work even harder to make pharmacy benefits easier for you and your members in the years to come.
A Timeline of COVID-19 Developments in 2020. American Journal of Managed Care. https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020. Published January 1, 2021. Accessed June 23, 2021.
Berry CR, Fowler A, Glazer T, Handel-Meyer S, MacMillen A. Evaluating the effects of shelter-in-place policies during the COVID-19 pandemic. Proceedings of the National Academy of Sciences. 2021;118(15). https://doi.org/10.1073/pnas.2019706118. Published February 24, 2021. Accessed June 23, 2021.
Panchal N, Kamal R, Cox C, Garfield R. The Implications of COVID-19 for Mental Health and Substance Use. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/. Published February 10, 2021. Accessed June 23, 2021.
Frequently Asked Influenza (Flu) Questions: 2020-2021 Season. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/season/faq-flu-season-2020-2021.htm#Flu-and-COVID-19. Updated February 18, 2021. Accessed June 23, 2021.
Beroukhim Afrahimi S. Flu numbers are down this year due to higher vaccination rates amid COVID pandemic. ABC News. https://abcnews.go.com/Health/flu-numbers-year-due-higher-vaccination-rates-amid/story?id=74783195. Published December 18, 2020. Accessed June 23, 2021.
[Sassy_Social_Share]
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.