Trend Over Time: Saving Money Isn’t a Race, It’s a Marathon
Partnering with the right pharmacy benefit manager (PBM) is about more than year-one savings. It’s about finding a PBM that truly understands and aligns with a payer’s needs, now and in the future.
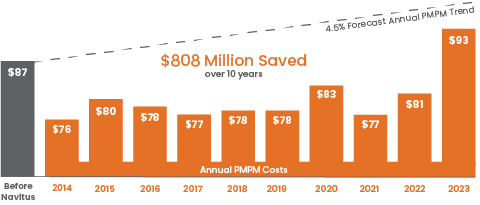
10+ Years of Savings
One of our clients, Self-Insured Schools of California (SISC), partnered with us in 2014, as they wanted to offer stable, affordable benefits to the school districts under their umbrella of service.
We were able to lower costs, without sacrificing quality of care, by:
- Implementing a custom, high-performance formulary to mitigate waste
- Eliminating more than 600 unnecessary drugs
- Enacting a comprehensive prior authorization (PA) process and a step therapy program to support lower-cost treatment options
As a result, SISC saw a 13.4% decrease in total net cost per member per month (PMPM) spend in their first year. And in the decade since, SISC has achieved $808 million in savings and has had more than 26 million claims processed. More importantly, in an industry where costs continue to increase year over year, SISC has seen minimal increases to its pharmacy benefit costs, with an average total net cost PMPM of $80.15 over 10 years. This is less than their PMPM in 2013.
Negative Trend for Five Years Straight
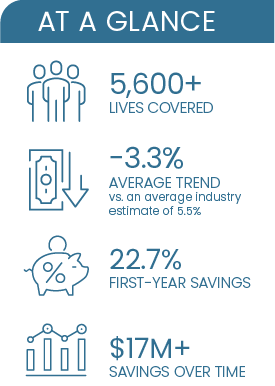
Another client, a regional building materials supplier, partnered with us in 2020. We were able to not only save them millions in the first year alone but also keep them at a negative trend over the following years.
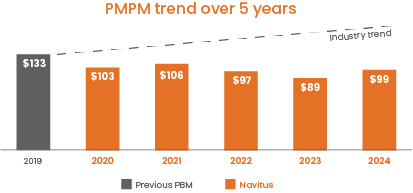
We accomplished all this and more by implementing:
Our lowest-net-cost formulary – We create efficient formularies that are clinically effective and limit waste, leading to the lowest net cost while maintaining high quality of care.
Our pass-through model – Our completely transparent model means that our clients pay what we pay and immediately receive 100% of the discounts that we negotiate on their behalf, eliminating spread pricing and rebate chasing.
The Lumicera cost-plus specialty pharmacy and a preferred pharmacy network – As one of the few cost-plus pharmacies in the nation, Lumicera clients only pay the invoiced actual drug acquisition cost, plus a flat patient-management fee and shipping. Lumicera is also well-regarded for its high-touch support model that offers patients education, personalized guidance and ongoing assistance.
See how we’re helping our partners achieve their long-term goals by downloading our 2024 Drug Trend Report.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








