Taking the Unnecessary Costs Out of Pharmacy Benefits
Identifying Opportunities for Savings
Concerned about growing prescription expenses, the State of Montana (the State) knew it was time for a change. With its traditional pharmacy benefit manager (PBM), costs reached levels equating to almost 20% of its total plan spend. This triggered its search for a fully-transparent PBM who could help manage its growing prescription costs.
The State knew the importance of finding a long-term PBM partner that was progressive, attentive to its needs and offered a 100% transparent pass-through model with a focus on delivering the lowest net cost. Through the evaluation process, the State identified substantial savings opportunities available through a PBM partnership with Navitus.
Developing a Better Pharmacy Benefits Plan
The partnership led to better-managed prescription costs and improved member health. With a focus on fine-tuning its formulary management, networks and specialty pharmacy approach, the State was able to improve performance and effectively reach its goals.
Improving Formulary Management Performance
A newly established formulary provided access to high-quality, clinically-effective mediations to improve health and deliver the lowest net cost. State members were grandfathered anywhere from three months to one year to help them adjust to the new formulary. The State was able to use a comprehensive, clinically-focused prior authorization (PA) process and step therapy program to support lower cost alternatives, while ensuring members received the most clinically-appropriate, safe and cost-effective medications.
Creating Network Savings
A limited network helped the State lower costs and increase savings opportunities. Members were encouraged to use key pharmacies to optimize discount rates and reduce dispensing fees. With the potential savings opportunities, combined with convenient pharmacy locations and access to extended day’s supply, members experienced minimal disruption and were able to transition prescriptions to the limited network pharmacies with ease.
Implementing a High-Touch Specialty Pharmacy Program
With specialty drug utilization increasing, a cohesive specialty pharmacy program was essential to help better manage expenses in this high-cost segment. Lumicera Health Services, Navitus’ wholly-owned subsidiary, served as the preferred specialty pharmacy where members received the lowest copay on specialty medications. For drug not available at Lumicera, members were eligible to get their medication for the same copay at other preferred specialty pharmacies within network.
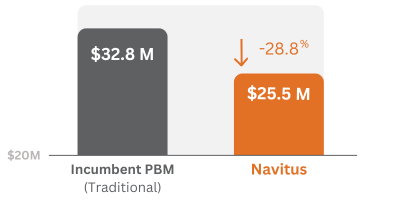
Achieving Double-Digit Savings
The implementation of these programs and other cost-reduction strategies resulted in a 28.8% decrease in total net cost in the first year. Navitus’ unique pass-through model guaranteed 100% of all discounts and rebates received were passed directly back to the state.
Since transitioning to Navitus, the State:
- Achieved $2 million in formulary savings, with no changes in utilization
- Retained $6.1 million in rebates, up from $1.2 million — 100% of which was passed directly to the State
- Realized a total net cost per member per month (PMPM) of $73.91 as compared to the industry average of $90.66
- Decreased member cost share by 5%
- Received approximately $2.5 million more in subsidies by transitioning from Retiree Drug Subsidy (RDS) to Medicare Part D Employer Group Waiver Plan (EGWP)
Total Net Cost In First Year
Why Switch from RDS to EGWP?
- Plan receives 100% of rebates, coverage gap discounts and CMS subsidies
- No pharmacy spread or risk premium
- Potential savings over RDS of up to 25%
Getting Started
Are you interested in finding out how Navitus’ transformative pass-through approach can work for you? Contact us at [email protected] to find out how you can take back control and start saving on your pharmacy benefits today!
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








