Turning Data Into Insights: Addressing Social Determinants of Health
Shed light on the socioeconomic factors that may be affecting member health and start taking action. Find out how in today’s blog!
WHAT ARE SOCIAL DETERMINANTS OF HEALTH?
Social determinants of health (SDOH) are the conditions in the places where people live, learn, work and play that affect a wide range of health and quality-of-life outcomes and risks.1
Approximately 68% of people have at least one SDOH challenge.2 Research suggests SDOH drive more than 80% of health outcomes, and medical care alone has shown to be insufficient at improving member health.2
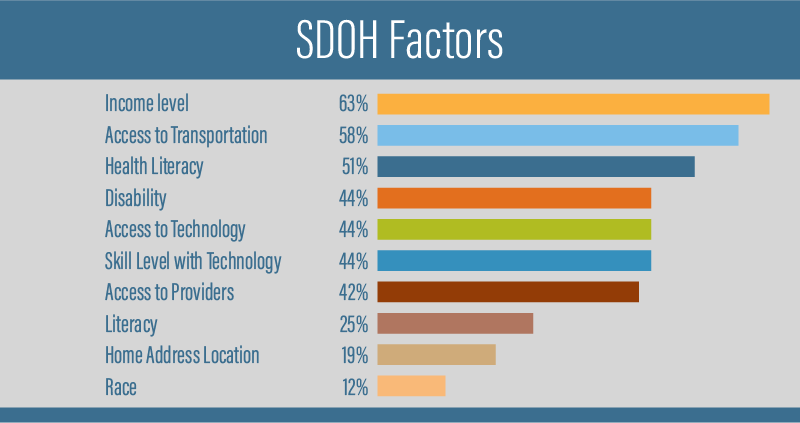
In a recent survey, providers cited a number of SDOH factors as having a significant effect on health care access, including income level, transportation availability, health literacy, home environment and access to providers.3
Pharmacy benefit managers (PBMs) have a unique opportunity to help plan sponsors identify and address SDOH using data, analytics and coordination of care. Let’s examine the five key areas of SDOH and explore a few tips to help members overcome challenges along their health care journey.

Economic Stability
The economic fallout of the pandemic resulted in millions of people losing their jobs and potentially their primary source of income. Many people were faced with sacrificing essential needs to afford medications or foregoing treatment altogether to pay bills.3
Tip #1:
Consider leveraging predictive analytics to help identify medication non-adherence, improve clinical outcomes and reduce health care expenditures.
Navitus’ Predictive Analytics Reporting uses many variables, including sociodemographic data, to identify members who would benefit from outreach and discussions on the importance of taking medications regularly. The additional clinical support can address gaps in care early on and help the member avoid complications that can lead to costly medical expenses such as emergency room visits and hospital stays, while improving members’ overall condition management.
Education Access & Quality
It’s important for plan sponsors to understand how to educate members on their benefits using a variety of communication methods, including verbal, printed and electronic. Ensuring members have access to adequate resources and can easily understand their benefits will help improve health literacy and overall health.
Tip #2:
With many people working from home or social distancing in the workplace, plan sponsors may have had to reconsider how to best communicate employee benefits. Here are a few tips and strategies to effectively communicate benefits in this new era.

Health Care Access & Quality
According to a recent report, national health care spending is expected to reach $6.2 trillion by 2028.4 As costs continue to rise, it becomes increasingly important to pursue opportunities that can address or eliminate barriers to receiving health care services.
Digital health options such as mobile health, wearable devices, telehealth and health information technology can provide members with a variety of options to receive high-quality health care in alternative ways.
Tip #3:
Navitus offers an extensive suite of evidence-based digital therapeutics programs to help members manage a range of conditions to improve health outcomes and lower costs.
Neighborhood & Built Environment
The neighborhoods people live in can have a major impact on their health and overall well-being. For example, individuals who live in rural areas may have limited access to transportation for health care needs. Addressing individual surroundings or barriers to care can help identify opportunities to promote better health.

Tip #4:
Navitus’ Clinical Engagement Center (CEC) helps members overcome health care challenges and address barriers to health through personalized clinical support. The CEC assesses SDOH and identifies opportunities to intervene and improve health outcomes. These pharmacist-led interventions can enhance the patient-care team relationship through deepened conversations that will help members better manage their chronic condition and medications.

Social & Community Context
Interventions to help people get the social and community support they need are an important factor to improving health and well-being. While many people face challenges beyond their control, creating a positive and healthy work environment, free of discrimination, can have a positive impact on daily life.
Start engaging with your members to improve health outcomes and lower pharmacy benefit costs today! Contact your account representative or email [email protected] to learn how Navitus’ robust suite of clinical programs can help.
Social Determinants of Health. Healthy People 2030, U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Published 2020. Accessed November 25, 2020.
Geneia. Addressing the Real Implications of Social Determinants of Health. Health Payer Intelligence. https://healthpayerintelligence.com/news/addressing-the-real-implications-of-social-determinants-of-health. Published April 1, 2019. Accessed February 3, 2021.
2021 Medication Access Report. CoverMyMeds. https://insights.covermymeds.com/medication-access-report?utm_medium=external&utm_source=guest-post&utm_campaign=mar-21&utm_term=drugchannels&utm_content=sponsored-link. Published January 29, 2021. Accessed February 15, 2021.
National Health Expenditures 2019 Highlights. Center for Medicare & Medicaid Services. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHe althExpendData/NHE-Fact-Sheet. Published December 16, 2020. Accessed February 15, 2021.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Examining Trends that Drive Informed Decisions
Now Available: 8th Annual Drug Trend Report
See the latest results and access industry insights you need to navigate current trend drivers.








