Fact or Myth: The Truth Behind a Lowest-Net-Cost Approach to Manage Rx Spend
Did you miss last month’s World Congress webinar? Keep reading to get a recap!
Faced with the economic pressures from the COVID-19 pandemic, prescription affordability and pharmacy benefit spend is under the microscope. Plan sponsors are searching for a better way to manage costs while preserving quality care for their members.
During the World Congress webinar last month, Navitus’ Bob Zakrajsek and Thomas Radloff shared their invaluable insight on key components plan sponsors should consider when trying to control their pharmacy benefit spend.
After a short introduction of Navitus Health Solutions and how we differ in the industry, Bob asked the audience the following poll question: “Is your PBM contract based on a traditional, hybrid or pass-through business model?” Audience results showed 35% partner with a pass-through PBM, 32% are with a traditional PBM, 22% didn’t know and 11% were with a hybrid PBM.
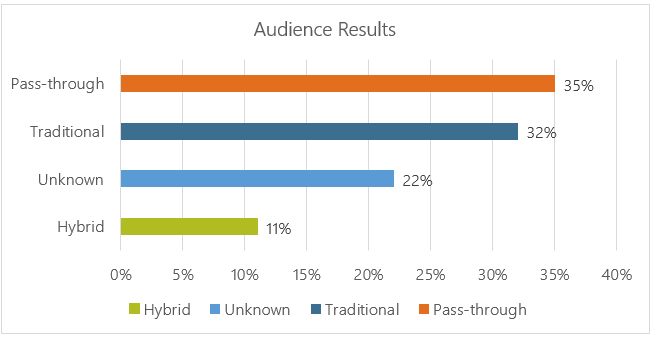
Key takeaway: If you don’t know what business model your PBM partner uses, you may be spending more than you should.
Understanding PBM Business Models
Bob provided a high-level overview of PBM models, varying degrees and definitions of transparency across those models and how that can affect plan spend.
Pass-through PBMs focus on the pass through of costs and revenue back to plan sponsors. This model is fully transparent, so the PBM’s business practices and all fees and charges are visible. Bob shared that,
“We as a PBM operate with only one administrative fee and no additional margins…our clients and book of business metrics consistently show that our lowest-net-cost approach, coupled with our thoughtful and effective clinical utilization management solutions drive saving and performance.”
He explained that discounts and rebates are inaccurate ways to truly measure costs. It’s most important to focus on the per member per month (PMPM) fee to ensure you’re not overpaying for your pharmacy benefits.
“Aligned incentives should be more than just a description in your business model and it should really be a foundation of how you operate your business. [Tom] will talk about some of the strategies and really how to obtain results from your formulary.”
Tom began by emphasizing that while all Navitus’ formularies are customizable and all drugs are available for a formulary, it’s what you do with those drugs that drives savings. Here are the three key components to consider to create a strong formulary foundation:
ENSURE PRODUCTS PROVIDE EVIDENCE-BASED, CLINICAL VALUE. All drugs should be reviewed for efficacy. At Navitus, only those that are found effective remain on the formulary.
MANAGE TO THE OVERALL LOWEST NET COST. Focus on low-cost generics and less expensive brands that consistently deliver the lowest net cost and reduce PMPM expenses.
MYTH: OFTEN TIMES HIGHER-COST DRUGS COME WITH THE BIGGEST REBATES AND GENERATE MORE “SAVINGS.”
FACT: WITH A FOCUS ON GENERICS AND LESS EXPENSIVE BRANDS, INITIAL REBATES APPEAR TO BE LOWER. HOWEVER, THE OVERALL SAVINGS IS ACTUALLY HIGHER.
Tom explained that, “We firmly believe in generics first, in all potential categories where that fits in, but we also look at where those formulary brands apply as well.”
APPLY UTILIZATION MANAGEMENT TOOLS. Along with ensuring the formularies consist of effective drugs and managing to the lowest net cost, it’s important to apply utilization management tools to ensure product use reaches the highest level of value. Examples include prior authorization (PA), step therapy and quantity limits.
While selecting a formulary that aligns with your company’s goals is important, it is crucial that the transition from one formulary to another is a positive experience for members. That’s where Navitus’ Clinical Engagement Center (CEC) comes in.
Delivering Personalized Clinical Care
This program focuses on these four areas:
MEDICARE MEDICATION THERAPY MANAGEMENT (MTM) is a requirement of Medicare Part D. This program improves member health outcomes with comprehensive medical reviews and person-to-person consultations.
ACADEMIC DETAILING is an educational outreach to prescribers by pharmacists in regards to prescribing habits.
PERSONALIZED MEMBER TRANSITIONS is for new members who will have a formulary change. Members will receive a letter that outlines the transition, they will receive a phone call to discuss formulary alternatives and our staff will contact prescribers to obtain new prescriptions.
STARS SUPPORT is a clinical outreach to support Medicare Star ratings.
Tom added, “It really creates a positive and seamless member experience. It’s all about member satisfaction. They have really enjoyed the communication that we are having with our team as part of that, and it really reduces those gaps in care that we have seen and smooths out those transition processes when we have new clients that come on board and/or when we add or modify drugs on our formulary.”
Bob concluded the webinar by stating, “At the end of the day, I think it is about making informed decisions.”
Making Informed Decisions
It is important to understand how your PBM operates. Think about discussing with your PBM:
Costs that will incur over the contract life
Pricing practices the PBM has in place
Ways to control costs
And, you may want to consider:
Transparent PBMs that offer flexibility and the ability to customize all aspects of your plan
Reducing wasteful drug spend with formulary management and utilization management programs
Understanding contractual definitions
Ensuring you have full access to your data and audit it down to the claim
Want more tips on how to control your pharmacy spend? Listen to the full webinar here.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.








