Driving Down Costs & Improving Health with Effective Diabetes Management Strategies
Looking for ways to trim your pharmacy benefit costs and improve member health? Diabetes is a good place to start.
Diabetes is a common chronic disease affecting more than 34 million adults in the United States today, with 90% of those cases being type 2 diabetes.1 Moreover, about 88 million Americans are pre-diabetic. Given the increasing incidence of this condition and the costs to effectively manage it, plan sponsors can expect this chronic condition to impact their benefit costs for years to come.
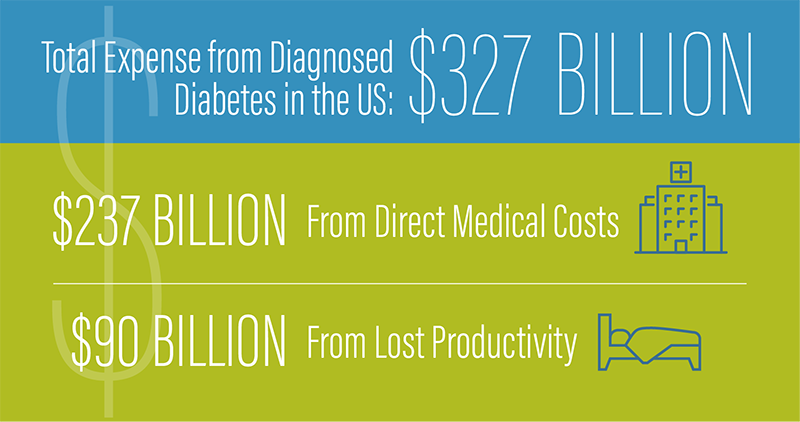
Speaking of costs, according to the American Diabetes Association (ADA), the total expense from diagnosed diabetes in the U.S. is $327 billion, including $237 billion from direct medical costs and $90 billion from lost productivity.2
FACING ONGOING CHALLENGES
Members diagnosed with diabetes have an uphill struggle complying with a complicated daily management regime. This includes carefully monitoring diet, blood sugar levels and exercise. To add to it, consistently taking prescribed therapies poses yet another challenge. According to the Association of Diabetes Care and Education Specialists3:
Half of all individuals with chronic diseases do not take their medications as prescribed
About 30% of individuals with diabetes report missing at least one dose of oral antihyperglycemic medication each month
More than 20% of new prescriptions for chronic conditions are never filled
Additionally, overall health care costs for a person with diabetes can be burdensome, with yearly medical costs averaging $16,752.4 An individual’s income level can also impact abandonment rates for medications. For example, diabetes medications costing $125 to $250 have an abandonment rate of 40% for households with an annual income of $100,000 and nearly 50% for households with an income of $25,000 or less.5
GAINING GREATER CONTROL WITH PROVEN STRATEGIES
To effectively manage one of the most widespread and costly conditions, plan sponsors need strategies to specifically address the most common diabetic needs. Once properly addressed through ongoing support and management, plan sponsors can expect to see improved health outcomes and lower costs. Navitus offers several solutions, including:
Pharmacoadherence
For members with diabetes, medication adherence is essential to improving outcomes and reducing complications, hospitalizations and ER visits. However, barriers to medication adherence can include forgetfulness, limited knowledge, physician-related issues such as poor communication and financial burden. Our Pharmacoadherence program identifies members who are chronically non-adherent, likely to become non-adherent or who never pick up a newly prescribed medication. Once a member is identified, intervention letters are mailed to members and their physicians. These communications include information about care coordination and education, while encouraging medication adherence. In our most recent data, 47% of members who we contacted through this program experienced improved adherence.

Diabetes Care Optimization
Getting medications and support to individuals diagnosed with type 2 diabetes as soon as possible is critical to improving health outcomes and lowering costs. Through our Diabetes Care Optimization program, we conduct a retrospective claims analysis review to identify members with type 2 diabetes who are taking insulin and other diabetes medications. Actionable reporting is provided to plan sponsors with clinical staff to assist with case management and provide assistance in obtaining prescriptions for metformin, which is recommended by the ADA, if medically appropriate. This medication can help lower the use of more expensive diabetes medications and improve member health.
Digital Therapeutics
Managing diabetes is complex and can be overwhelming, especially for those newly diagnosed. Health care apps are widely used and, when combined with the support of a member’s health care team, can improve outcomes and save plan costs. Plan sponsors and members can benefit from our BlueStar® digital therapeutics app, which supplements existing care for members with diabetes. This app engages members with personalized, real-time feedback and education to help them take charge of their diabetes. Members can track activity, medication, labs, diet and symptoms.

Members can also share this data with their care team, helping their prescribers track member health and make more informed decisions. For patients with type 2 diabetes, BlueStar has demonstrated an average 2% reduction in hemoglobin A1C levels and can result in cost savings of 58% from reductions in hospitalizations and ER visits.
To learn more about how our programs can deliver plan savings and help your members effectively manage their diabetes, email or contact your account team today!
Diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/basics/type2.html. Accessed February 15, 2021.
American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917-928. doi:10.2337/dci18-0007.
Fostering Medication Taking Tips and Tricks. Association of Diabetes Care & Education Specialists. https://www.diabeteseducator.org/docs/default-source/living-with-diabetes/tip-sheets/medication-taking/fostering_med_adherence.pdf?sfvrsn=4. Accessed February 16, 2021.
What to Do When You Can’t Afford Your Diabetes Medication or Supplies. ADW Diabetes. https://www.adwdiabetes.com/articles/afford-diabetes-medication-supplies. Accessed February 18, 2021.
Medicine Spending and Affordability in the United States. IQVIA Institute for Human Data Science. (2020). https://www.iqvia.com/en/insights/the-iqvia-institute/reports/medicine-spending-and-affordability-in-the-us. Published August 4, 2020. Accessed February 15, 2021.
Health Dialog. The Roadmap to Medication Adherence: 6 Critical Steps That Drive Success.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Examining Trends that Drive Informed Decisions
Now Available: 8th Annual Drug Trend Report
See the latest results and access industry insights you need to navigate current trend drivers.








