Reducing Costs and Improving Service
Overcoming Pharmacy Benefit Challenges
Over time, one university grew increasingly dissatisfied with the service level it was receiving from its traditional pharmacy benefit manager (PBM). Despite the long-term relationship with its PBM, something needed to change.
Located in the Midwest, the university desired to find a PBM partner that was local, collaborative and allowed it to be involved in its pharmacy benefit decisions. This included finding a PBM solution to lower its pharmacy benefit costs and provide its members with superior service. Its desire for improved service, for members and at the account level, was a key factor for consideration during the evaluation process.
Finding a Long-Term PBM Partner
With high expectations, the university collaborated with its consultant to evaluate a number of PBMs that could deliver on its needs. After thorough evaluation, it decided to move forward with a partnership with Navitus. Several factors contributed to its decision, including the quality of service, cost savings, opportunities and location.
Even within the early stages of implementation, the level of service the university began to receive far exceeded its expectations. The university knew this was the beginning of a long-term PBM partnership.
Improving Client and Member Service
In an effort to improve both client and member service, the following initiatives took place.
Implementing Effective Communication: To introduce the new plan, members received robust onboarding communications through various methods, including a welcome letter, an employee health and wellness fair, benefit newsletters and a custom benefit enrollment website. The customized benefit enrollment website allowed its members to preview their plan design options, formulary documents and cost compare tool prior to going live with Navitus.

Lowering Pharmacy Costs: To mitigate member cost concerns for diabetes medications at retail pharmacies, Navitus incorporated a modified plan design for the university that allowed members to bypass the deductible an receive insulin products at a lower cost at the point-of-sale. This reduced a significant cost barrier that members were previously experiencing, and allowed members to receive additional savings while promoting effective health management.
Working Collaboratively: Navitus provided benefit and program recommendations to the university’s own task force committee, which made all pharmacy benefit decisions. The teams also collaborated during monthly status meetings to monitor progress and discuss pharmacy benefit initiatives continue to enhance plan performance. This collaboration allowed the university to be involved in its pharmacy benefit decisions and continue to provide the best offerings for its members.
Achieving Significant Savings
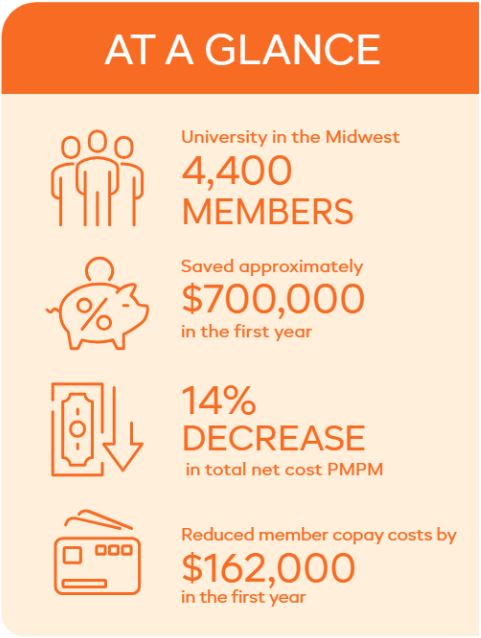
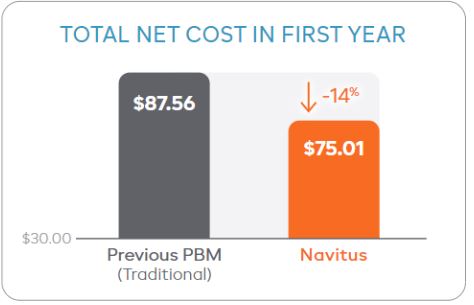
After transitioning to Navitus, it did not take long for the university to begin seeing significant savings. In the first year, its total net cost per member per month (PMPM) went from $87.56 with it previous PBM, down to $75.01, a 14% decrease.
Using a conservative forecast trend of 0.5%, the university saved an estimated $12.99 total net cost PMPM for the first year by transitioning to Navitus. This equates to approximately $700,000 in savings.
Looking forward, the university plans to take advantage of mail order service to offer additional savings to members without limiting the network. With the new mail order option, members will benefit from mail order discounts with a convenient 90-day supply, and enhanced pricing on extended days’ supply medications at certain retail pharmacies. This will allow the university to take advantage of a more cost-effective channel, while providing enhanced benefits and cost savings opportunities for its members.
Getting Started
Are you interested in finding a long-term PBM relationship and a solution to lower your pharmacy benefit costs? Contact us at [email protected] to find out how you can start saving today!
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.