Prior Authorization
Prior Authorization: What is It and How Does It Affect Me?
Prior authorization (PA) is one of the many tools that support our mission to improve member health and lower costs. It’s a standard health care process that most pharmacy benefit managers (PBM) use to ensure you’re taking safe, cost-effective medications.
Prescriptions may need prior authorization if they:
- Could be unsafe if taken with other drugs
- Are often misused or abused
- Have more affordable, effective alternatives
How It Works
Drugs that need prior authorization are listed on your formulary with a PA.
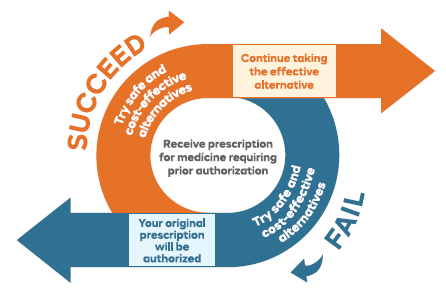
If a drug requires prior authorization, more information is usually required from your prescriber before the prescription can be filled. You also may be asked to try an alternative prescription that’s already covered, if your diagnosis or situation allows.
When an alternative isn’t effective or is advised against, we’ll partner with your prescriber and plan sponsor to find a solution and get you the care you need.
Rules around prior authorization are informed by the U.S. Food and Drug Administration (FDA), your plan sponsors and the Navitus Pharmacy and Therapeutics Committee, with the goal of helping you get safe and affordable medications that work.
We know how important timely access to your medication is, so most prior authorization requests are reviewed within two business days and urgent requests within one business day.
Stay Informed and Connected
Receive expert insights, healthcare tips, and important updates on pharmacy benefits, drug recalls, and more—straight to your inbox.
Navigating with a trusted partner
Now Available: 9th Annual Drug Trend Report
Our Drug Trend Report provides a clear view of the trends shaping pharmacy benefits today, along with strategies that are delivering real savings without compromising care.







